Cognitive dysfunctions are a core feature of schizophrenia and have been shown to play a major role in the functional outcome of the disorder.1
Overall functioning is strictly tied to quality of life. Functional impairment in schizophrenia is largely caused by negative and cognitive symptoms, which can affect social functioning, working memory and executive function. It is important for modern drug regimens to address this critical unmet need.
Despite the amount of data supporting the benefits of cognitive remediation interventions in schizophrenia, a number of questions remain to be answered. Identification of potential predictors of effectiveness of cognitive rehabilitation is at the forefront of research, because the efficacy of treatments largely depends on the appropriate selection of individuals, depending on the severity of the disease and treatment methodologies.2
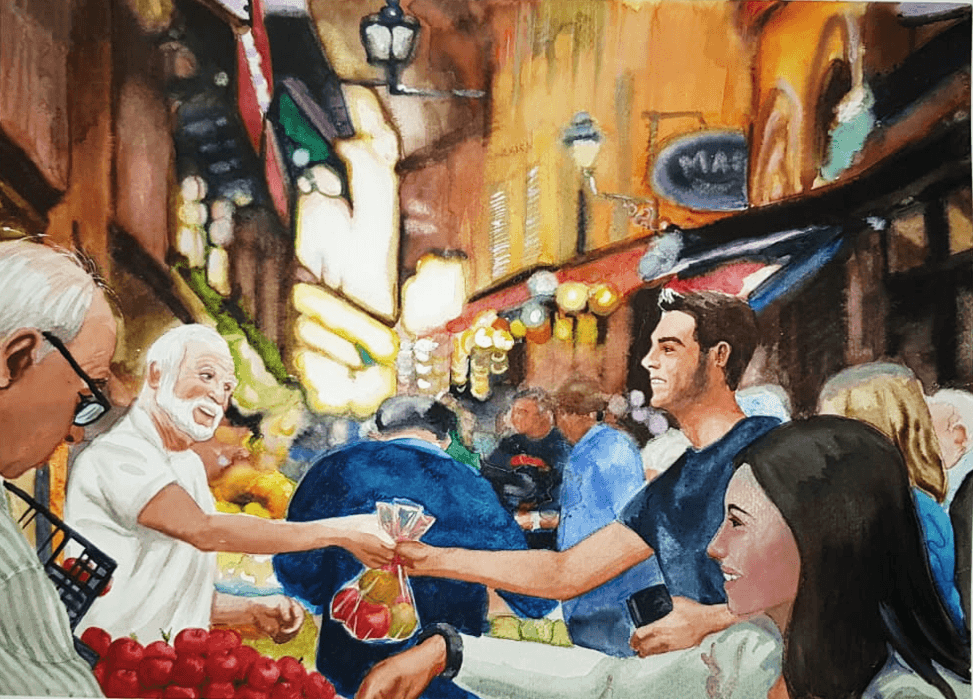
There’s a lesser discussed therapeutic objective when treating schizophrenia. It goes beyond reducing frequency of psychotic episodes, and it’s often not as well targeted as positive symptoms: functioning.1
Improving an individual’s functional capacity will affect their quality of life, which is ultimately, as valuable as treating positive symptoms. A multi-modal approach to treatment will normally encompass psychopharmacology, psychosocial interventions and assistance with housing and financial sustenance.3
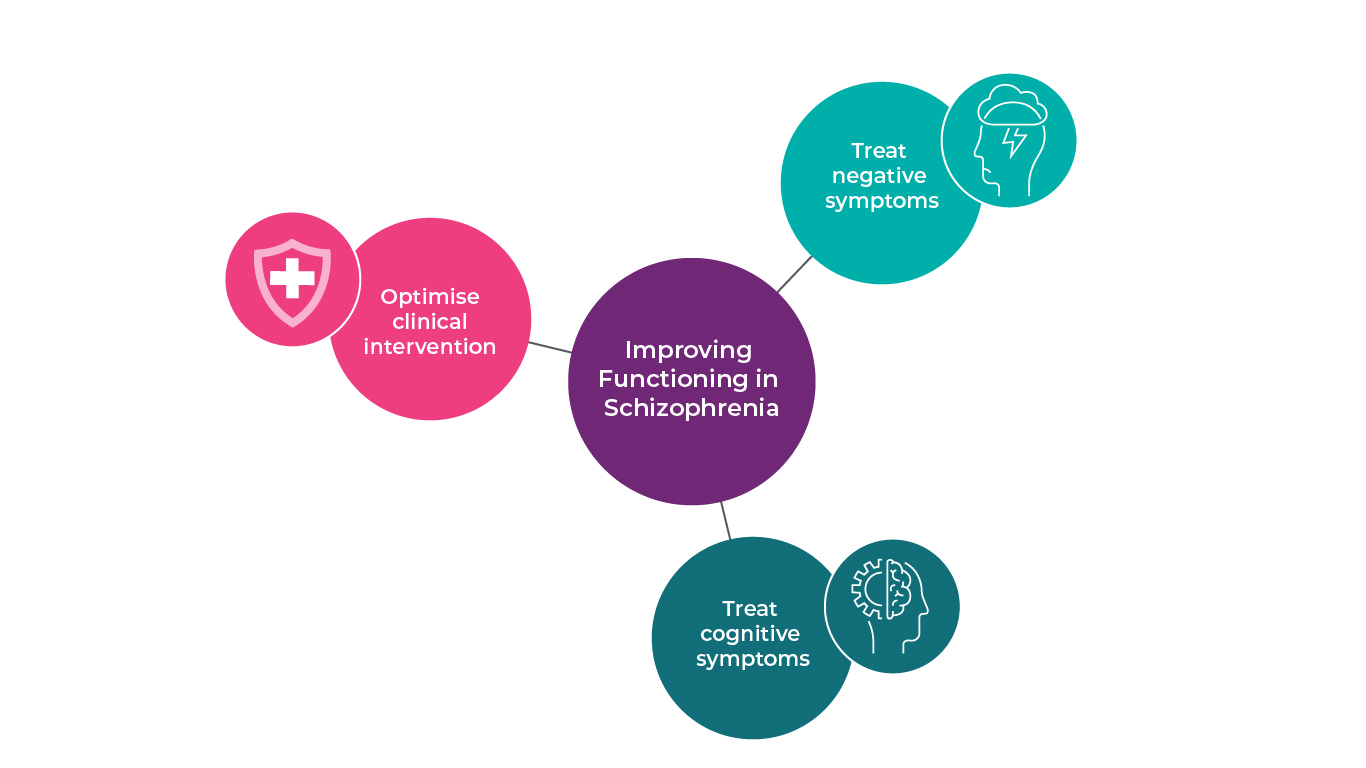
It’s crucial to adapt and personalise the clinical intervention (Fig 1). Monitoring the individual, the clinical progress made, and considering changes to the treatment regimen would positively contribute to medication adherence, therapeutic efficacy and continuity of care.4
There are several interventions available, depending on the case and the severity of the disease.
Acute psychotic episodes
In an acute psychotic episode, the most important thing is the reduce positive symptoms. In these cases, adequate pharmacotherapy is the number one choice, considering functionality as well. It is crucial to choose a medication that wouldn’t sedate or cause unbearable side effects to the patients, as potential “iatrogen” disadvantageous factors in terms of functionality. It is safer to achieve sedation with benzodiazepines, by administering the lowest effective dose, rather than antipsychotics. Choosing a highly sedating antipsychotic drug at this stage can impede discharge later. 5
Chronic psychotic episodes
Positive symptoms are treated similarly across the diagnoses, although different dose levels, schedules, and durations are used. However, when acute psychotic symptoms are not that often or present, but negative symptoms and cognitive symptoms dominate the clinical picture, there is room for other kind of interventions. Cognitive behavioural therapy, for example, is recommended as a first-line intervention for the treatment of mild to moderate depression and anxiety.6 In such cases, adaptation of a healthy lifestyle and regular exercise are also highly recommended, as they have been proven toameliorate brain function by improving memory, multi-tasking and planning, induces brain cell repair and lengthens the attention span.7 Finally, financial support and fulfilling career aspirations are crucial to maintain remission.
Even though the process of such interventions is not always described clearly, each type of intervention model has an individual set of goals and objectives, as well as a treatment agenda, and all have been found to be effective in improving different aspects of the functioning of patients with schizophrenia. However, there are difficulties in implementing these interventions in everyday clinical practice in community care settings, such as insufficient resources to deliver and evaluate the selected intervention adequately, limited number of caregivers or inadequate training to them and insufficient recognition and support in existing mental health services.8
Treating negative symptoms is also a key element to consider when looking at improved functioning (Fig 1).3 Although negative symptoms affect up to 26% and 58% of schizophrenia patients and outpatients, respectively, they respond less well to current medications than positive symptoms.9 Furthermore, only a few antipsychotics have evidence for being effective in negative symptoms.10 For this reason, the lack of efficacious treatments for negative symptoms remains a significant unmet need, especially considering the importance of these symptoms on patient outcomes.9 It is therefore crucial to recognise, understand and tackle negative symptoms promptly, as early intervention can greatly affect overall functioning and, subsequently, quality of life.8
Alongside negative symptoms, there’s another class of symptoms with no approved targeted treatment: cognitive symptoms (Fig 1). These are also linked to overall functioning and remain an unmet medical need.11,12 Cognitive symptomatology includes poor executive functioning, especially in decision-making and elaborating information, attention deficits and reduced working memory.13 Plausibly, these symptoms are likely to affect patients’ quality of life and daily functioning. Research into cognitive symptoms has progressed considerably in the last few decades. Nevertheless, modern drug targets and regimens still struggle to achieve considerable improvements in this class of symptoms. Successful pilot trials targeting cognitive symptoms have failed to be replicated in larger trials. This demonstrates that ample research on the topic is still critical.14
The main therapeutic goal of today’s drug regimens is to enhance overall functioning, and yet, most clinical improvements are largely found in tackling positive symptoms. Modern treatment options should include a focus on negative and cognitive symptoms, be reviewed frequently and consistently, and adapted according to the individual’s needs and preferences.15 A successful antipsychotic regimen should, ideally, integrate treatment of all class of symptoms, enhance social functioning and prevent further cognitive impairment. The biggest indication of a highly successful treatment plan should be a noticeable improvement in overall functioning, leading to an enhanced quality of life.16
References
- Bowie et al. Am. J. Psychiatry. 2006; 163 (3): 418–425
- Medalia and Richardson. Schizophr. Bull. 2005; 31 (4): 942–953
- Haller CS. F1000Prime Reports 2014;6:57
- NICE Psychosis and schizophrenia in adults: prevention and management 2014
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1839209/pdf/bmj-334-7595-cr-00686.pdf
- https://www.nasmhpd.org/sites/default/files/DH-CBTp_Fact_Sheet.pdf Cognitive Behavioral Therapy for Psychosis (CBTp): Fact Sheet, Hardy K, Stanford University Department of Psychiatry and Behavioral Health
- EPA Report(27th European Congress of Psychiatry) 2019
- Chien et al. Neuropsychiatric Disease and Treatment. 2013; 9: 1463–1481
- Chue P, Lalonde JK. Neuropsychiatr Dis Treat. 2014 May 8;10:777-89. doi: 10.2147/NDT.S43404. Review
- Krause, M., Zhu, Y., Huhn, M. et al. Eur Arch Psychiatry Clin Neurosci (2018) 268: 625
- Carbon M. CNS Spectr 2014;Suppl 1:38-52
- Buchanan RW. Schizophr Bull 2007;33: 1013–1022
- National Institute of Mental Health. Schizophrenia. 2009
- Goff DC. Pharmacol Biochem Behav 2011;99(2):245–253
- Carbon M, Correll CU. Dialogues Clin Neurosci. 2014 Dec;16(4):505-24. Review. PubMed PMID: 25733955; PubMed Central PMCID: PMC4336920.
- Sommi, 2017 (https://www.medscape.org/viewarticle/463775)
what is schizophrenia? Quick overview of schizophrenia
Schizophrenia can be defined as a severe mental disorder which affects behaviours, thoughts and emotions. You may only notice the first symptoms around teenage Schizophrenia can be defined as a severe mental disorder which affects behaviours, thoughts and emotions. You may only notice the first symptoms around teenage
more...studying and working with... studying and working with...
People with long-term mental health conditions, including schizophrenia, experience barriers to work, due to stigma, prejudice, and discrimination. Despite the People with long-term mental health conditions, including schizophrenia, experience barriers to work, due to stigma, prejudice, and discrimination. Despite the
more...